
Důkazem vysokého vzdělání je schopnost mluvit o největších věcech nejjednodušším způsobem.
David Hume
Výzkum
Relevance of infection with human papillomavirus (HPV) - the role of p53 tumour suppressor protein and E6/E7 zinc finger proteins
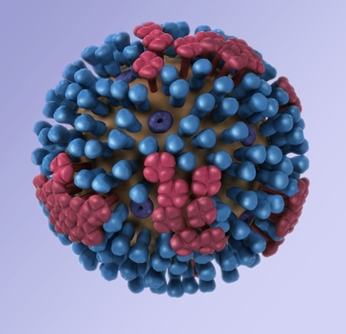 Papillomavirus is a DNA virus that causes benign and malignant epithelial growths. Grigorieff and Harrison used cryo-EM to show that neighboring pentamers in its icosahedral shell exchange “invading arms” to form a stable and rigid capsid. Credit: Wolf, M., Garcea, R. L., Grigorieff, N. & Harrison, S. C. (2010) Subunit interactions in bovine papillomavirus. PNAS, 107, 6298–6303.
Papillomavirus is a DNA virus that causes benign and malignant epithelial growths. Grigorieff and Harrison used cryo-EM to show that neighboring pentamers in its icosahedral shell exchange “invading arms” to form a stable and rigid capsid. Credit: Wolf, M., Garcea, R. L., Grigorieff, N. & Harrison, S. C. (2010) Subunit interactions in bovine papillomavirus. PNAS, 107, 6298–6303.
Human papillomaviruses (HPVs) are a large family of small double-stranded DNA viruses that infect squamous epithelia [1].
HPV has been accepted as an etiologic agent for cervical carcinoma and the first association with head and neck cancer was published in 1985 [2]. HPV was also shown to play a role in the pathogenesis of a subset of head and neck squamous cell carcinomas (HNSCCs) [3]. Almost 650 000 patients worldwide are diagnosed with head or neck cancer each year and 350 000 patients die of this disease. [2]. Oral cancer is the sixth most prevalent type of cancer worldwide. The ratio of males to females is approximately 2:1 [4]. Papillomaviruses infect and cause papillomas in most mammals [5, 6]. The viruses are absolutely species-specific [1] and they have been detected in a variety of mammalian and avian species including humans, parrots, canines and felines [7]. The term head and neck cancer includes malignancy in an area that comprises the skin, oral cavity, salivary glands, lip, pharynx, larynx, nasal cavity, paranasal sinuses and soft tissues of the neck and ear [4]. The majority of these malignancies are HNSCC [4, 8, 9]. Two types of clinical precancer lesions have been established: white lesions (leukoplakia) and reddish lesions (erythroplakia) [10]. Precancerous lesions of the oral mucosa are epithelial changes that are able to undergo malignant transformation more likely than normal tissue at other mucosal sites. HPV is also a central causative agent in cervical carcinogenesis [11]. HPV selectively infects the epithelium of the skin and mucous membranes. Specific HPV types are associated with squamous cell carcinoma, adenocarcinoma, and dysplasias of the cervix, penis, anus, vagina, and vulva [12]. Up to now, 150 HPV genotypes have been identified and fully sequenced [13-15].
 Determination of HPV genotype is based on the degree of homology within the L1 (major capsid protein) ORF [13]. If the DNA sequence of the L1 ORF differs by more than 10% from the closest related known type, it is regarded as a novel type. HPV types associated with skin warts are for example HPV-1, 2, and 4 [16]. A wide range of HPV types including HPV-5, 8, 9, 23 and 47 cause epidermodysplasia verruciformis lesions, which can be transformed to malignancy upon exposure to ultraviolet light [17]. The largest subgroup is represented by HPV types infecting mainly mucosal surfaces of the genital and respiratory tracts. More than 40 of the identified HPV types belong to this group [13]. HPV types are often referred to as “low-risk“ or “high-risk“ based on their potential for oncogenesis. The high risk HPV types include HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, -68, -73, and -82. The ‘‘low-risk’’ HPV types cause especially benign lesions affecting the anogenital areas, such as genital warts (condylomata), low-grade squamous intraepithelial lesions (SILs) of the cervix, and laryngeal papillomas. These low-risk types include HPV-6, -11, -40, -42, -43, -44, -53,-54, -61, -72, and -81[18].
Determination of HPV genotype is based on the degree of homology within the L1 (major capsid protein) ORF [13]. If the DNA sequence of the L1 ORF differs by more than 10% from the closest related known type, it is regarded as a novel type. HPV types associated with skin warts are for example HPV-1, 2, and 4 [16]. A wide range of HPV types including HPV-5, 8, 9, 23 and 47 cause epidermodysplasia verruciformis lesions, which can be transformed to malignancy upon exposure to ultraviolet light [17]. The largest subgroup is represented by HPV types infecting mainly mucosal surfaces of the genital and respiratory tracts. More than 40 of the identified HPV types belong to this group [13]. HPV types are often referred to as “low-risk“ or “high-risk“ based on their potential for oncogenesis. The high risk HPV types include HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, -68, -73, and -82. The ‘‘low-risk’’ HPV types cause especially benign lesions affecting the anogenital areas, such as genital warts (condylomata), low-grade squamous intraepithelial lesions (SILs) of the cervix, and laryngeal papillomas. These low-risk types include HPV-6, -11, -40, -42, -43, -44, -53,-54, -61, -72, and -81[18].
Podpořeno projekty: SPINCANCER
Plakáty k výzkumným směrům
Dokumenty pro VaV aktivity
Výzkumný záměr
Hodnocení výzkumných aktivit
Archív
21— 2013 20— 2013 19— 2013 18— 2013 17— 2013 16— 2013 15— 2013 14— 2013
 | Zemědělská 1/1665 613 00 Brno Budova D | Tel.: +420 545 133 350 Fax.: +420 545 212 044 |  |
 |





